Abstract
The Biopharmaceutical Classification System (BCS) has been a prognostic tool for assessing the potential effects of formulation on the human drug oral bioavailability. When used in conjunction with in vitro dissolution tests, the BCS can support the prediction of in vivo product performance and the development of mechanistic models that support formulation assessments through the generation of “what if” scenarios. To date, the applicability of existing human BCS criteria has not been evaluated in dogs, thereby limiting its use in canine drug development. Therefore, we examined 50 drugs for which absolute bioavailability (F) was available both in dogs and humans. The drugs were also evaluated for any potential association between solubility (calculated from the dose number, Do) or lipophilicity (LogP) and F in dogs. In humans, solubility is determined in 250 mL of fluid. However, the appropriate volume for classifying drug solubility in dogs has not been established. In this analysis, the estimated volume of a water flush administered to fasted dogs (6 mL) and a volume of 250 mL scaled to a Beagle dog (35 mL) were examined. In addition, in humans, a Do value greater than 1.0 is used to define a compound as highly soluble and a LogP value greater than 1.72 as high permeability. These same criteria were applied for defining highly soluble and highly permeable in dogs. Whether using 35 or 6 mL to determine Do, the canine solubility classification remained unchanged for all but seven compounds. There were no clear associations between a drug’s F in dogs and humans or between the canine value of F and either its human BCS classification, its LogP value, or the canine Do estimate. There was a tendency for those drugs with canine values of F equal to or greater than 80% to have LogP values equal to or greater than 1.0. Exceptions to this observation tended to be those compounds known to be absorbed via mechanisms other than passive diffusion (e.g., via transporters or paracellular transporters). Although there are limitations to the approach used in this study, the results of our assessment strongly suggest that the human BCS classification system requires substantial modification before it can be reliably applied to dogs.
INTRODUCTION
The United States Pharmacopeial Convention (USP) authorized the creation of an advisory panel to investigate the possibility of applying the principles of the Biopharmaceutics Classification System (BCS) to veterinary drugs—specifically, solid oral formulations administered to dogs (1). Developed for human pharmaceutical compounds (–), the BCS is an important tool that facilitates product development and regulatory decisions. By understanding the solubility of a compound in biorelevant media and its permeability across biological membranes, the rate limiting factors determining the rate and extent of oral drug absorption can be identified. This information can be invaluable for predicting the potential influence of formulation and physiological variables on oral drug bioavailability.
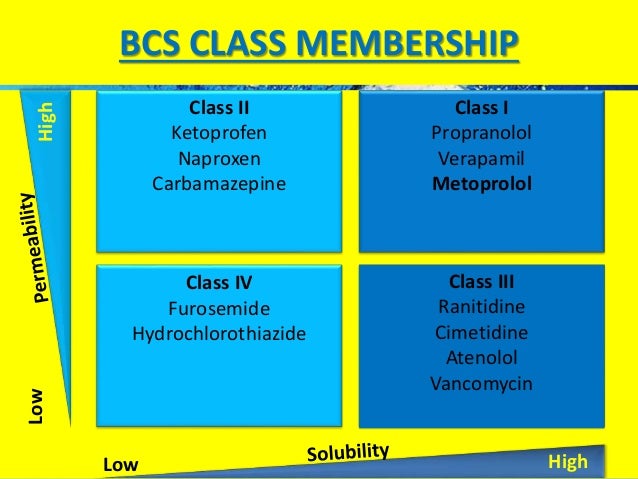
Within the framework of human pharmaceuticals, drugs can be classified into one of the following four BCS categories:
Class I: high solubility, high permeability: generally very well-absorbed compounds
Class II: low solubility, high permeability: exhibits dissolution rate-limited absorption
Class III: high solubility, low permeability: exhibits permeability-limited absorption
Class IV: low solubility, low permeability: very poor oral bioavailability
A complementary classification system was proposed by Wu and Benet (, ). They recognized that drugs exhibiting high permeability are generally extensively metabolized, while poorly permeable compounds are primarily eliminated as unchanged drug in the bile and urine. Thus, the Biopharmaceutical Drug Disposition Classification System (BDDCS) has been used to predict drug disposition and potential drug-drug interactions in the intestine and the liver and potentially the kidney and brain. Although the solubility criteria for the BCS and BDDCS are the same, there is a substantial difference in the second variable being considered. For the BDDCS, the second classification is related to the extent of drug metabolism. Conversely, the assessment of permeability in the BCS is linked to the extent of intestinal absorption, i.e., a drug is considered to be highly permeable when the extent of the systemic absorption (parent drug plus metabolites) in humans is determined to be at least 90% of an administered dose based on a mass balance determination or in comparison to an intravenous reference dose. Accordingly, the BCS and BDDCS classification of a drug may differ.
The US Food and Drug Administration’s (FDA’s) Center for Drug Evaluation and Research (CDER) (9) has incorporated BCS concepts into guidance documents for human medications into the 2000 FDA Guidance for Industry, including guidance for the waiver of in vivo bioequivalence study requirements for high solubility/high permeability drug products. However, the BCS has not as yet been extrapolated for application to veterinary drugs. The reason for this gap is that the BCS was developed based upon human digestive physiology, which can be vastly different from that observed in veterinary species. Given the similarity of therapeutic entities used in the dogs and humans, and because of the use of the dog as a preclinical species for human medicine (), it would be of particular value to have an understanding of how the BCS criteria can be translated between human and canine gastrointestinal (GI) physiologies.
The solubility criteria used both by the BCS and the BDDCS rely upon formulation considerations in that it is based upon the highest dose that will be administered. Both the BCS and the BDDCS define a high solubility compound at the highest marketed dose strength that is soluble in 250 mL of water over the pH range of 1–7.5 at 37°C. This definition differs from that of “intrinsic solubility,” which reflects the equilibrium aqueous solubility of a compound. For acids and bases, intrinsic solubility represents the concentration of the unionized species in a saturated solution at the pH value where that compound is fully unionized (). While there has been some debate regarding certain compounds whose intrinsic solubility may not be accurately defined when using conventional media (, 13), those considerations are founded upon the perspective of a drug’s physicochemical characteristics rather than on the in vivo conditions into which that drug will be introduced. Thus, while intrinsic solubility is solely a function of the molecule, the BCS (or BDDCS)-based solubility criteria is dependent upon physiological conditions and the corresponding targeted therapeutic dose. Unfortunately, what constitutes the BCS-based criteria for high or low solubility is currently undefined for dogs because of complexities associated with interspecies differences in the composition of the GI milieu (1).
Another obstacle confronted when trying to establish canine-specific BCS criteria is the challenge associated with the classification of intestinal permeability. Despite the range of high throughput systems available for examining human intestinal permeability, such as Caco-2 cells, parallel artificial membrane permeability assay (PAMPA), and phospholipid vesicle-based permeation assay (PVPA), these methods for estimating drug permeability have only been applied to human drugs (, ). These systems have not been developed and validated for application to drug permeability across the canine intestine (, ). Moreover, while one may argue that transcellular permeability should be similar in humans and dogs, the GI tract of the dog tends to be more permeable (leakier) because of the larger intercellular pores ().
Currently, the existing in vitro methods for evaluating drug permeability have not succeeded in providing data that can be extrapolated to dogs. For this reason, we needed to resort to comparisons based upon the use of absolute bioavailability. Because there are no suitable in vitro methods to assess effective permeability in dogs (Peff), we have used absolute bioavailability (F) for this analysis. We have justified this approach because a comparison of drug absorption across human colonic epithelium cell layers (Caco-2 cell line) to absorption across canine colon tissue did not show a relationship (). The Ussing chamber technique, which has been evaluated for other veterinary species (), has not been applicable for canine studies () because of the fragility of the tissue. Membrane damage that occurs prevents permeability measurements using this technique in dogs (). Therefore, without the availability of these in vitro tools, other data must be used to predict permeability and apply BCS criteria for oral drugs administered to dogs.
The current investigation was undertaken because of the lack of established BCS criteria to evaluate oral medications administered to dogs. The objectives were to examine the properties that define human BCS criteria for drugs and to compare this information to pharmacokinetic data available from studies in dogs. Without in vitro intestinal permeability data in dogs, another parameter must be considered to classify a drug as either high or low permeability. To this end, there are numerous molecular factors that impact drug transcellular permeability, including hydrogen bonding properties, molecular size and shape, polarity, flexibility, and ionization properties (, ). There is no “gold standard” or [even a suggested criterion based upon the log of the lipophilicity coefficient (LogP) pH-dependent lipophilicity value (LogD)] that has been proposed as a cutoff value. Therefore, we focused on the use of the systemic absorption value (absolute bioavailability, F), which we were able to obtain from the published literature. It was assumed that if the value of F is high, permeability (via active or passive processes) must likewise be high. We also acknowledged at the outset that the converse was not necessarily true and that the use of F as an indicator of drug permeability will produce some false negative results, i.e., there are drugs that have high permeability, but low values of F because of other factors such as intestinal efflux or high first-pass metabolism.
A drug solubility classification has not been established for medications administered to dogs (, 25). To classify a drug as either high or low solubility in dogs requires that one knows the ideal volume in which to measure solubility. In this study, we have examined two different volumes and considered whether this parameter can be useful to predict oral absorption of medications in dogs.
Ultimately, the objective of this study was to identify the in vitro drug properties with respect to their potential impact on dog-human differences and similarities on oral drug solubility and permeability. The foundational assumption was that if properties can be identified, we could then generate dog-specific criteria for applying BCS concepts to understand the critical formulation and physiological variables that can influence canine oral drug absorption. Similar to its tremendous influence on human drug product development and regulatory evaluation, a roadmap for screening oral product formulations, if applied to veterinary drug products, would provide a tool for screening new formulations. Additional benefits that would be associated with a canine-specific BCS would be an improvement on our ability to compare human formulations for potential testing and clinical use based upon information obtained in dogs (and vice versa).
One of our objectives was to extend our assessment beyond the results reported by Chiou et al., () in which the oral bioavailability of 43 compounds was compared in humans and dogs. In that study, they observed that while 22 of the 43 compounds were completely absorbed in both humans and dogs, the overall interspecies correlation of F values was low (coefficient of determination, R2 = 0.51). A pitfall associated with the investigation by Chiou et al. was that much of the data were based upon radiolabeled data, thereby precluding a differentiation between parent compound and metabolites. Given the potential for interspecies differences in intestinal metabolism, and since F values were based on total urinary recovery of radioactivity of the drug (thereby further confounding the comparison with potential differences in post-absorption processes), we could not use that information to generate predictions on the permeability component of the BCS. However, we also recognized that a drug with a high first-pass effect may be reported with high F in the study by Chiou et al. (), but not in our study reported. Thus, in addition to evaluation of BCS classification versus F in dogs and humans, we compared our F values with those reported by Chiou et al. ().
EXPERIMENTAL METHODS
To explore the potential application of BCS principles for oral drugs administered to dogs, pharmacokinetic, lipophilicity, and solubility data were either calculated or were obtained from existing literature. Lipophilicity, calculated as the octanol / water partition coefficient (LogP) was used to estimate permeability because there is no in vitro permeability data available for dogs, we used the experimental LogP values (which consider the ratio of unionized solute concentrations in octanol versus that in water), rather than Log D (which is ratio of the concentration of drug in octanol versus the sum of the concentration of both the neutral and ionized moieties in water) primarily because we found the LogP values to be more readily available for all 50 compounds in our study and because LogP had previously been included as a surrogate for predicting the intestinal permeability for human drugs (–). The list of drugs for which human BCS criteria were already derived was used as a starting database (–). Values for current BCS classification, solubility (expressed as mg/mL), and LogP were obtained from an internet web site that lists these criteria (Therapeutic Systems Research Laboratories (TSRL), Inc; http://tsrlinc.com/resources/services/) (27). Solubility data (mg/mL) and LogP estimates were also obtained from the literature (–). From the hundreds of drugs listed in the references cited above, the literature was searched for data on oral absorption of those compounds for which we were able to obtain data in dogs. The F values for dogs were obtained from published sources, the manufacturer’s data (approved drug label), or in some instances from the author’s unpublished research. Although we found additional published information on the oral bioavailability for some veterinary drugs (), human data and human BCS criteria were not available for these veterinary-specific drugs, and therefore, these compounds were excluded from our analysis.
With respect to classification of drug solubility, one of the challenges was the absence of the ideal canine gastric volume that can be used for estimating a dose number (Do). The Do used in the calculations for determining BCS criteria is determined by the formula:
where M is the dose strength of the tablet/capsule, V is the volume administered (defined as 250 mL for humans), and C is the drug’s solubility (mg/mL).
A volume of 250 mL, the typical volume of water consumed during human bioavailability studies, is too large to be appropriate to estimate the volume of water flush administered to a fasted dog. Therefore, other volumes were explored for the calculation of a Do. In one analysis, we used a volume of 6 mL because this is often the volume administered to dogs with an oral medication (a single “flush” with a 6-mL syringe). A volume of 6 mL also has been suggested as the residual volume in the empty canine stomach (1, , 25). Additional analysis was performed using 35 mL because it is equivalent to the 250 mL (~ one cup) when scaled to the size of an average Beagle dog (the breed used most often in oral drug absorption studies).
The relationships between canine estimates of F versus human BCS values, solubility, LogP, Do, and F values for humans were compared by linear regression. This was accomplished using the Proc Reg procedure in SAS (version 9.3). Both slope and intercepts were included in the regression equation. Confidence and prediction intervals about the regression line were set at alpha = 0.10 (90% intervals, 5% in each tail). The regression of Do on F was expressed relative to the natural logarithm of Do (LD). This evaluation was conducted both at Do values estimated at a volume of 6 mL (LD6) and 35 mL (LD35).
RESULTS
Oral absorption data were obtained for 50 drugs for which human and canine data were available (–; Papich, 1986, Pharmacokinetics of ranitidine and cimetidine in dogs, unpublished data; –; Papich, 1988, Pharmacokinetics of doxycycline in dogs after intravenous administration and oral administration of doxycycline hyclate and doxycycline monohydrate, unpublished data; –; Papich, 1986, Pharmacokinetics of lorazepam in dogs, unpublished data; –). Four drugs had conflicting data and therefore were listed twice to include both sets of data. For two drugs (, ), publications addressing BCS biowaivers for human formulations had data that conflicted with an official web site (27) or other published data (–). These drugs were listed twice to accommodate both data. Many of these drugs were administered to dogs as the human formulation or as a compounded product when there was no approved veterinary counterpart. For two drugs (furosemide and phenobarbital), two sets of canine values were considered because of duplication of published data. There was a relatively even distribution of drugs among the four BCS classes. There were 16 drugs from class I, 9 drugs from class II, 15 drugs from class III, and 10 drugs from class IV. As a percentage of drugs, this was a higher representation of class III and class IV drugs than the analysis of Takagi et al. ().
Table I summarizes the information used in our examination of the relationships between drug physicochemical parameters and the oral absorption performance in humans and dogs. For consistency, we relied primarily upon two sources of information for the BCS classification: Kasim et al. (), using their LogP-based estimates for our predictions of drug permeability, and Wu and Benet (). For those several compounds that were not contained within those two references, other published values were used (, , , ). Despite recognized diversity in some of the values across these various information sources, we concluded that since the magnitude of differences was small relative to the overall strength of the trends that were observed, any error that may have been introduced by the selection of publications would not influence the conclusions derived from our comparison.
Table I
Analysis of 50 Drugs in Humans and Dogs Using Solubility, Lipophilicity, and Comparison of Bioavailability (F), According to BCS Class (Four Drugs Are Listed Twice Because of Two Sets of Conflicting Data)
| Drug name | Max dose (mg) human | Intrinsic solubility (mg/mL) | Do | LogP | F human | BCS class | Dose dogs (mg) | F (dog) | Do (35 mL) dogs | Do (6 mL) dogs | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Acetaminophen | 500 | 0.1 | 20 | 0.89 | 0.87 | 4 | 140 | 0.63 | 40.000 | 233.333 | () |
| Amlodipine | 10 | 1 | 0.04 | 0.29 | 0.74 | 3 | 25 | 0.63 | 0.72 | 4.16 | () |
| Amoxicillin | 500 | 4 | 0.5 | −0.58 | 0.93 | 3 | 272 | 0.768 | 1.94 | 11.33 | () |
| Atenolol | 100 | 26.5 | 0.015 | 0.16 | 0.54 | 3 | 400 | 0.83 | 0.43 | 2.52 | () |
| Azithromycin | 600 | 0.01 | 240 | 4.02 | 0.34 | 2 | 240 | 0.97 | 685.71 | 4000 | () |
| Bisoprolol | 10 | 1000 | 0.00004 | 1.94 | 0.8 | 1 | 11 | 0.914 | 0.00031 | 0.002 | () |
| Carvedilol | 25 | 0.01 | 10 | 3.14 | 0.25 | 2 | 11 | 0.143 | 31.43 | 183.33 | () |
| Cephalexin | 500 | 1 | 2 | −0.67 | 0.95 | 4 | 240 | 0.57 | 6.86 | 40.000 | () |
| Chlorpheniramine | 4 | 100 | 0.00002 | 3.77 | 0.41 | 1 | 100 | 0.36 | 0.029 | 0.17 | Papich, 1986, Pharmacokinetics of ranitidine and cimetidine in dogs, unpublished data,() |
| Cimetidine | 800 | 6 | 0.53 | 0.79 | 0.62 | 3 | 96.25 | 0.95 | 0.46 | 2.67 | () |
| Cimetidine | 800 | 6 | 0.53 | 0.79 | 0.62 | 3 | 100 | 0.75 | 0.48 | 2.78 | (, ) |
| Ciprofloxacin | 750 | 10 | 0.3 | 1.32 | 0.6 | 4 | 250 | 0.584 | 0.71 | 4.17 | () |
| Clindamycin | 300 | 100 | 0.012 | 2.16 | 0.87 | 1 | 150 | 0.7255 | 0.043 | 0.250 | () |
| Clomipramine | 25 | 100 | 0.001 | 5.65 | 0.48 | 1 | 56.2 | 0.16 | 0.016 | 0.094 | () |
| Codeine | 60 | 100 | 0.0024 | 1.45 | 0.5 | 3 | 45 | 0.04 | 0.013 | 0.075 | () |
| Cyclosporine | 100 | 0.01 | 40 | 2.95 | 0.28 | 2 | 50 | 0.35 | 142.86 | 833.33 | (43) |
| Diazepam | 10 | 1 | 0.04 | 2.98 | 1 | 1 | 40 | 0.146 | 1.1429 | 6.67 | () |
| Diltiazem | 120 | 100 | 0.0048 | 2.64 | 0.38 | 1 | 30 | 0.26 | 0.01 | 0.050 | () |
| Digoxin | 0.25 | 0.01 | 0.1 | 1.95 | 0.7 | 1 | 0.36 | 0.58 | 1.029 | 6.000 | () |
| Dolasetron | 100 | 100 | 0.004 | 0.062 | 0.068 | 1 | 65 | 0.07 | 0.019 | 0.11 | () |
| Doxycycline | 100 | 0.1 | 4 | −3.66 | 0.93 | 4 | 100 | 0.365 | 28.57 | 166.67 | Papich, 1988, Pharmacokinetics of doxycycline in dogs after intravenous administration and oral administration of doxycycline hyclate and doxycycline monohydrate, unpublished data |
| Doxycycline | 230.8 | 33 | 0.028 | −3.66 | 0.93 | 1 | 100 | 0.365 | 0.08 | 0.49 | () |
| Fluoxetine | 50 | 10 | 0.02 | 4.27 | 0.95 | 1 | 20 | 0.72 | 0.057 | 0.33 | (49) |
| Furosemide | 80 | 0.01 | 32 | 0.74 | 0.61 | 4 | 400 | 0.77 | 1142.86 | 6666.67 | () |
| Furosemide | 80 | 0.01 | 32 | 0.74 | 0.61 | 4 | 40 | 0.383 | 53.33 | 666.67 | () |
| Gabapentin | 800 | 100 | 0.032 | −1.12 | 0.6 | 3 | 850 | 0.8 | 0.24 | 1.42 | () |
| Hydralazine | 50 | 40 | 0.005 | 0.73 | 0.35 | 3 | 104 | 0.77 | 0.074 | 0.43 | () |
| Hydroxyzine | 100 | 0.01 | 40 | 3.32 | 0.6 | 2 | 42.5 | 0.72 | 121.43 | 708.33 | () |
| Ibuprofen | 800 | 0.01 | 320 | 3.14 | 0.8 | 2 | 87.5 | 0.77 | 250.00 | 1458.33 | () |
| Ketoprofen | 75 | 0.051 | 5.9 | 3.31 | 0.9 | 2 | 100 | 0.9 | 56.022 | 326.80 | () |
| Levetiracetam | 750 | 1040 | 0.0029 | 2.79 | 1 | 1 | 500 | 1 | 0.014 | 0.080 | () |
| Linezolid | 600 | 1 | 2.4 | 0.58 | 1 | 4 | 250 | 0.966 | 7.14 | 41.67 | (, ) |
| Lorazepam | 2 | 0.08 | 0.1 | 2.39 | 0.93 | 2 | 9.4 | 0.598 | 3.36 | 19.58 | Papich, 1986, Pharmacokinetics of lorazepam in dogs, unpublished data |
| Meloxicam | 15 | 0.01 | 6 | 0.97 | 0.97 | 2 | 2.55 | 1 | 7.29 | 42.50 | () |
| Metoclopramide | 10 | 0.01 | 4 | 1.48 | 0.82 | 3 | 23 | 0.478 | 65.71 | 383.33 | () |
| Metronidazole | 500 | 10 | 0.2 | −0.46 | 0.99 | 1 | 435.6 | 0.8 | 1.25 | 7.26 | () |
| Minocycline (HCl) | 100 | 50 | 0.01 | 0.05 | 0.95 | 3 | 100 | 0.503 | 0.08 | 0.5 | () |
| Morphine | 10 | 62.5 | 0.001 | 1.19 | 0.24 | 3 | 15 | 0.053 | 0.007 | 0.040 | () |
| Naproxen | 500 | 33 | 0.06 | 2.86 | 0.99 | 1 | 100 | 0.84 | 0.087 | 0.51 | () |
| Phenobarbital | 100 | 0.1 | 4 | 1.52 | 1 | 1 | 133.65 | 0.88 | 38.19 | 222.75 | () |
| Phenobarbital | 100 | 0.1 | 4 | 1.52 | 1 | 1 | 364.5 | 0.97 | 104.14 | 607.50 | () |
| Phenytoin | 100 | 0.01 | 40 | 2.14 | 0.9 | 2 | 155 | 0.36 | 442.86 | 2583.33 | () |
| Piroxicam | 20 | 0.023 | 3.48 | 3.06 | 0.9 | 2 | 4.2 | 1 | 5.22 | 30.44 | () |
| Procainamide | 500 | 5 | 0.4 | 0.88 | 0.83 | 3 | 250 | 0.85 | 1.43 | 8.33 | () |
| Propranolol | 90 | 33 | 0.01 | 2.65 | 1 | 1 | 10 | 0.27 | 0.009 | 0.051 | () |
| Ranitidine | 300 | 100 | 0.012 | 0.63 | 0.27 | 3 | 38.5 | 0.81 | 0.011 | 0.064 | Papich, 1986, Pharmacokinetics of ranitidine and cimetidine in dogs, unpublished data |
| Rofecoxib | 50 | 0.01 | 20 | 1.83 | 0.93 | 2 | 50 | 0.26 | 142.86 | 833.33 | () |
| Sildenafil | 100 | 1 | 0.4 | 2.11 | 0.38 | 1 | 15 | 0.54 | 0.43 | 2.50 | () |
| Theophylline | 300 | 8.33 | 0.144 | −1.03 | 0.99 | 1 | 160 | 0.91 | 0.55 | 3.20 | (, ) |
| Tramadol | 50 | 33 | 0.006 | 2.52 | 0.73 | 1 | 87.8 | 0.65 | 0.076 | 0.44 | () |
Do dose number (defined in the text), LogP log of octanol/water partition coefficient, F systemic bioavailability, BCS class Biopharmaceutical Classification System class as defined in the references cited in the text
When assessing the relationship between estimates of F in dogs and humans (Fig. 1), we observed that the slope significantly differed from zero (P = 0.0055). However, the corresponding low coefficient of determination (R2 = 0.15) indicates that human estimates of F very poorly predicted canine F values. Without considering drug physicochemical characteristics, the potential contribution of drug solubility and/or permeability on the observed interspecies inconsistencies could be determined (and hence, the reason behind our further examination of these data). The intercept of the regression line was 0.31, which might be construed as suggesting a trend toward higher canine drug bioavailability when the human oral drug bioavailability is very low. Indeed, of the nine drugs with human estimates of F less than 0.40, six were associated with canine F values equal to or greater than that observed in humans. However, given the very low R2 value, such conclusions should be construed as an overinterpretation of the observed canine/human relationship. Along with this caution is the observation of wider confidence and predictions toward the intercept.
The relationship between oral bioavailability (F) observed in humans versus dogs. Although there was much variability in the relationship between estimated values of F in dogs and people, a statistically significant correlation was observed (p = 0.0055). The confidence interval (as defined by the shaded region around the regression line) reflects variability both in slope and intercept attributable to the uncertainty in the estimated regression line. While the wider prediction interval likewise reflects the uncertainty of the data, it predicts the interval within which the regression will be contained (90% of the time) if the analysis were repeated using a comparable human and canine populations (i.e., relating the prediction of dog F from human F). The intercept (dog F observed when the human F = 0) is 0.31, indicating an overall trend toward a higher bioavailability in dogs at very small human values of F. The slope of the regression of dog versus human is 0.42
Despite the low overall correlation between human and canine F values, when segregated according to its BCS class relationship, patterns begin to emerge (Fig. 2a–d). We observe that as compared to that observed in BCS classes III and IV, many of the compounds contained in BCS classes I and II demonstrated a good correlation between F in dogs and humans. In terms of the percent of the listed compounds where the human and canine F values differed by no more than +/−20%, these were found to be 79, 64, 36, and 20% for BCS classes I–IV, respectively (Table II). For BCS class I compounds, we observed a trend toward a lower bioavailability in dogs as compared to that in humans (Fig. 2a). Similarly, the class IV compounds tended to exhibit a comparatively lower oral bioavailability in dogs (Fig. 2d). For the nonsteroidal anti-inflammatory drugs (NSAIDs), all but one showed similar F values in dogs and humans (four were in class II or IV), which is consistent with their BCS classification of a low solubility compound being primarily a function of their behavior in acid. A surprisingly high number of drugs in class II (Fig. 2c) showed similar or higher F values in dogs compared to humans. Several of these compounds were weak bases.
Comparison of canine/human absolute bioavailability (F) as a function of human BCS classification: a BCS class I compounds, b BCS class II compounds, c BCS class III compounds, and d BCS class IV compounds. The hatched line represents the theoretical line of unity
Table II

Comparison of Drugs According to Bioavailability in Humans, Dogs, Therapeutic Class, pKa, and Metabolism
| Comparative F, dog versus humana | BCS | Drug | Human F (dose mg) | Dog F (dose mg) | Therapeutic class | pKa | First-pass loss | Cyp enzyme | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Similar | 1 | Bisoprolol | 0.8 (10) | 0.91 (11) | Beta-1 adrenergic blocker | 9.5 (base) | No | Cyp3A4, some Cyp2D6 | DrugBank |
| Similar | 1 | Chlorpheniramine | 0.41 (4) | 0.36 (100) | Alkylamine antihistamine | 9.2 (base) | Yes | CYP2D6 | http://cadd.suda.edu.cn/admet/compound/detail/573; () |
| Similar | 1 | Clindamycin | 0.87 (300) | 0.73 (150) | Lincosamide | 7.7 (base) | No | CYP3A4 | http://cadd.suda.edu.cn/admet/compound/detail/1350; Wynalda et al. () |
| Similar | 1 | Digoxin | 0.7 (0.25) | 0.58 (0.36) | Cardiotonic glycoside | – | No | Pgp may limit absorption. Minimal metabolism | http://www.rxlist.com/lanoxin-tablets-drug/clinical-pharmacology.htm |
| Similar | 1 | Diltiazem | 0.38 (120) | 0.26 (30) | Ca channel blocker | 7.7 (base) | Yes (Cyp3A4) | Cyp3A4 | DrugBank, druginfosys.com |
| Similar | 1 | Dolasetron | 0.068 (100) | 0.07 (65) | Serotonin 5-HT3 receptor antagonist | NA | Yes | CYP2D6, CYP3A4 | (43); http://cadd.suda.edu.cn/admet/compound/detail/878 |
| Similar | 1 | Levetiracetam | 1.0 (750) | 1.0 (500) | Anticonvulsant (binds to synaptic vesicle) | NA | No | Enzymatic hydrolysis | DrugBank, druginfosys.com |
| Similar | 1 | Linezolid | 1.0 (600) | 0.97 (250) | Anti-infective | 1.7 (base) | No | Primarily renal elimination of unchanged drug | (, ); http://www.fda.gov/ohrms/dockets/ac/00/backgrd/3597b1bb.pdf |
| Similar | 1 | Metronidazole | 0.99 (500) | 0.80 (435.6) | Antiprotozoal, antibacterial (anaerobe) | 2.6 (base) | No | Primarily CYP2A6, some CYP3A4, 5, and 7 | DrugBank, PharmacoKinetics Knowledge Base; () |
| Similar | 1 | Naproxen | 0.99 (500) | 0.84 (100) | NSAID | 4.15 (acid) | No | CYP2c8, 2c9, 1A2, UDP-glucuronosyltransferase | DrugBank |
| Similar | 1 | Phenobarbital | 1.0 (100) | 0.88–0.97 (133.65 to 364.5) | Nonselective central nervous system depressant | 7.3 (acid) | No | Mostly CYP2C19 | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 1 | Sildenafil | 0.38 (100) | 0.54 (15) | Phosphodiesterase type 5 inhibitor | 8.2 to 9.6 (base) | Yes | CYP3A4, also CYP2C9 | DrugBank, http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-Public_assessment_report/human/001080/WC500068025.pdf |
| Similar | 1 | Theophylline | 0.99 (300) | 0.91 (160) | Phosphodiesterase inhibitor | 8.6 (base) | No | CYP1A2 | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 1 | Tramadol | 0.73 (50) | 0.65 (87.8) | Opioid | 9.41 (base) | No | CYP3A4 and CYP2D6 | DrugBank, druginfosys.com |
| Not Similar | 1 | Clomipramine | 0.48 (25) | 0.16 (56.2) | Antidepressant | 9.38 | Yes | CYP2C19, CYP3A4, and CYP1A2 | DrugBank, PharmacoKinetics Knowledge Base, http://www.pharmgkb.org/pathway/PA165960076 |
| Not Similar | 1 | Diazepam | 1.0 (10) | 0.15 (40) | Benzodiazepine | 3.3 | No (human) | CYP2C19 and CYP3A4 | DrugBank, PharmacoKinetics Knowledge Base |
| Not similar | 1 | Doxycycline hylate | 0.93 (100) | 0.37 (100) | Tetracycline | 3.5, 7.7, 9.5 | No (human) | Negligible | http://cadd.suda.edu.cn/admet/compound/detail/1399 |
| NOT SIMILAR | 1 | Fluoxetine | 0.95 (50) | 0.72 (20) | Serotonin uptake inhibitor | 8.7 (base) | Yes | CYP2D6 | DrugBank, PharmacoKinetics Knowledge Base |
| NOT SIMILAR | 1 | Propranolol | 1.0 (90) | 0.27 (10) | Beta blocker | 9.5 | Yes (saturable) | CYP2D6, 1A2, and UGT | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 2 | Carvedilol | 0.25 (25) | 0.14 (11) | Beta blocker | 7.6 (base) | Yes | CYP2D6, CYP2C9 | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 2 | Cyclosporine | 0.28 (100) | 0.35 (50) | Immune-suppressant | 6.9 (base) | Yes | Cyp3A4 | (, ) |
| Similar | 2 | Hydroxyzine | 0.60 (100) | 0.72 (42.5) | Antihistamine | 1.8, 2.1, 7.1 | No | Cyp3A4/5 | Ucerax (hydroxyzine hydrochloride) 25 mg film-coated tablets. Summary of product characteristics. Irish Medicines Board. Retrieved 9 February 2014, http://web.squ.edu.om/med-Lib/MED_CD/E_CDs/A%20Practical%20Guide%20to%20Contemporary%20Pharmacy%20Practice/pdf/pKa-table.pdf |
| Similar | 2 | Ibuprofen | 0.80 (800) | 0.77 (87.5) | NSAID | 4.9 (acid) | No | CYP2C9 | http://cadd.suda.edu.cn/admet/compound/detail/277 |
| Similar | 2 | Ketoprofen | 0.9 (75) | 0.9 (100) | NSAID | 4.45 (acid) | No | Glucuronidation | DrugBank |
| Similar | 4 | Meloxicam | 0.97 (15) | 1.0 (2.55) | NSAID | 4.47 (acid) | No | CYP2C9 | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 2 | Piroxicam | 0.9 (20) | 1.0 (4.2) | NSAID | 6.3 (acid) | No | CYP2C9 | DrugBank |
| Similar | 3 | Amlodipine | 0.74 (10) | 0.63 (25) | Calcium channel blocker | 8.6 (base) | No | CYP3A4 | DrugBank, PharmacoKinetics Knowledge Base, http://www.pfizer.ca/en/our_products/products/monograph/212 |
| Similar | 3 | Amoxicillin | 0.93 (500) | 0.83 (400) | Beta lactam | 2.4, 7.4, 9.6 | No | Negligible | http://cadd.suda.edu.cn/admet/compound/detail/1089 |
| Similar | 3 | Cimetidine | 0.76 (800) | 0.95 n | H2-receptor antagonist | 6.8 (base) | No | Cimetidine/H+ exchange mechanism | Piyapolrungroj et al. () |
| Similar | 3 | Procainamide | 0.83 (500) | 0.85 (250) | Sodium channel blocker | 9.4 (base) | No | CYP2D6, CYP3A4 | DrugBank, PharmacoKinetics Knowledge Base |
| Similar | 4 | Ciprofloxacin | 0.60 (750) | 0.58 (250) | Antimicrobial | 6.09 (acid) and 8.89 (base) | No | Several (including CYP1A2) | DrugBank, PharmacoKinetics Knowledge Base |
BCS class Biopharmaceutical Classification System class as defined in the references cited in the text, F systemic bioavailability, Cyp enzyme cytochrome P450 enzyme, NSAID nonsteroidal anti-inflammatory drug
aDefinition of similar versus not similar: “Similar” is as any human/canine value of F that differed by no more than +/−20%. The 20% value was based upon the traditional bioequivalence (BE) criteria (linear scale) of equivalence being +/−20%. “Not similar” was defined as outside this range
As compared to that seen for BCS classes I and II, far fewer compounds exhibited comparable human versus dog bioavailability for BCS classes III and IV. With regard to the latter two classes, there was no obvious pattern identified such that very high or very low oral absorption could be correlated with values of F when comparing dogs to humans. For example, for class III drugs (Fig. 2c), there was somewhat of an even distribution above and below a line of unity. There were examples of some compounds that were more bioavailable in humans than in dogs (e.g., codeine), while others were more bioavailable in dogs than humans (e.g., ranitidine).
One of the potential sources of interspecies bias is the difference in gastric volume versus dose. For this reason, we estimated the Do, using a volume of 6 or 35 mL (representing a range of volumes administered in studies where dogs are administered a water flush after oral dose administration). As shown in Fig. 3a (6 mL volume) and b (35 mL volume), no obvious association between the calculated Do (expressed as LD) and F could be identified. This is evidenced both by low R2 values (0.031 and 0.029 and for 35 mL (LD35) and 6 mL (LD6), respectively) and the lack of statistical significance when evaluating the slope of the regression line (P = 0.23 and 0.22 for 3a and b, respectively), indicating that these slopes do not significantly differ from zero. Furthermore, the similarity in width of the confidence and prediction intervals at the upper and lower portions of the profile suggests that the error about the regression line is similar across the range of LD values obtained in this study.
The influence of the log-transformed dose number (LD) on the estimated value of F in dogs. a The relationship defined by volume of 6 mL (LD6). b The relationship defined by a volume of 35 mL (LD35). Interpretation of confidence versus prediction intervals corresponds with that previously described for Fig. 1
Figure 3a, b illustrates that regardless of whether a volume of 6 or 35 mL was used in the analysis, there was little influence of fluid volume on Do above, or below, 1.0. This indicates that either volume could adequately reflect oral dose solubility as a function of administered dose for most drugs administered to dogs. Using a Do of 1.0 as the cutoff between low and high solubility (as used for the human BCS), only seven drugs (gabapentin, cimetidine, amlodipine, ciprofloxacin, sildenafil, theophylline, and atenolol) would be classified as high solubility (Do < 1) using a volume of 35 mL, but low solubility (Do > 1) using a volume of 6 mL.
The influence of the lipophilicity (expressed as LogP) on F was examined in Fig. 4. When considering all of the drugs included in this analysis, no association could be identified between LogP and F (R2 = 0.0027). The large P value for the slope of the regression line (P = 0.72) indicates that the slope defining the regression of LogP on canine F is not significantly different from zero. Furthermore, similarities in the width of the confidence and prediction intervals at the upper and lower portions of the profile suggest that that the error about the regression line was similar across the range of LogP values. However, limiting our assessments to those drugs with F > 0.80 (Fig. 5), most had LogP values within the range of 0–4, suggesting transcellular absorption. The only compounds showing high F values but LogP < 0 in dogs were gabapentin, amoxicillin, metronidazole, and theophylline. The Do values in these four drugs ranged from below 0.001 to over 1000.
LogP value versus F value in dogs for 50 drugs. LogP is the experimentally determined lipid partition coefficient; the F value is the bioavailability in dogs. The estimated canine F value when LogP is zero is 0.62. The corresponding slope of the line is −0.008. The large P value indicates that this is not a significant correlation, and therefore, the negative slope should not be construed as being indicative of any true relationship. Interpretation of confidence versus prediction intervals corresponds with that previously described for Fig. 1
High bioavailability (approximately 80%) drugs in dogs compared to dose number and LogP. (Dose number and LogP were previously defined.) Four drugs (shown with open diamonds on the left side of the figure) were exceptions because they had LogP < 0, but good bioavailability: metronidazole, which is a small molecule absorbed paracellularly in dogs; gabapentin and amoxicillin, which are probably absorbed via intestinal transporters; and theophylline, which can be absorbed from the large intestine (colon)
To identify some commonality between agents exhibiting high human/canine correlations, we examined the pKa, mechanism of drug elimination (human), and whether or not a human first-pass drug loss was reported (Table II). The vast majority of compounds with similar values of F in dogs and humans were also those compounds with negligible first-pass drug loss. Furthermore, in the three out of four BCS class I compounds where human and canine F values were discordant, those compounds were reported to have a high human first-pass drug loss.
DISCUSSION
Whether we are providing values for F, solubility, permeability, or BCS classification, all values need to be viewed from the perspective as estimates derived under a specific set of experimental conditions. Thus, there are occasions where, for example, a compound was estimated as being within one BCS classification in one reference but as a different class for another reference (e.g., ciprofloxacin). The tables available from Takagi et al. () show some of these discrepancies. Similarly, values of F reported within this manuscript reflect a distinct set of experimental conditions, and therefore, there can be differences in reported estimates elsewhere, depending upon study conditions and population. For example, we can consider the compound amlodipine. In one study, the human oral bioavailability was stated to be 63% (). However, in the Pfizer monograph for amlodipine besylate (http://www.pfizer.ca/en/our_products/products/monograph/212), the absolute bioavailability of an oral administration ranged between 64 and 90%. Accordingly, on an individual compound basis, the estimated ratio of dog and human F values provided in this manuscript should be considered a single point within a distribution of potential estimates. That said, when viewed across a diverse library of compounds (as we have done in this manuscript), these values provide a tool for examining variables that can be used to examine interspecies relationships in drug absorption.
Highly soluble and highly permeable compounds will likely exhibit similar oral drug bioavailabilities unless the drug exhibits differing extent of first-pass metabolism in dogs versus humans. Nevertheless, we cannot conclude that a drug’s BCS classification will necessarily translate across species. BCS solubility classifications are traditionally based upon a calculation of the Do, which assumes a dissolution volume of 250 mL (approximately one cup of water). That volume is far greater than the gastric volume of the fasted dog. Typically, studies performed in dogs will include a water flush of 6 or 12 mL because, for practical reasons, these are common plastic syringe sizes. We included a high value of 35 mL in our analysis because this represents the equivalent to the 250 mL (~ one cup) in humans scaled to the size of an average Beagle dog (the breed used most often in oral drug absorption studies). Accordingly, compounds considered highly soluble in a human population may not meet the criteria for highly soluble in dogs. Regardless of whether we consider the canine gastric volume to be 6 or 35 mL, we found that the solubility classification would be affected for only a few compounds (Fig. 3a, b). Using a Do cutoff of 1.0 for distinguishing between low or high solubility compounds, only seven drugs, gabapentin, cimetidine, amlodipine, ciprofloxacin, sildenafil, theophylline, and atenolol, would have had a different solubility classification as a function of different volumes used for these calculations. In some cases, this solubility difference may impact oral drug absorption. For example, in the case of ciprofloxacin, Papich () observed that differences in the volume administered with the oral dose may indeed affect F in dogs. When ciprofloxacin tablets were administered with a volume that decreased the Do below 1, oral absorption was better than when the Do was >1. This observation points to the importance of dosing regimens and study design when interpreting study data.
Another challenge facing interspecies BCS extrapolations is that by convention, a drug is classified as highly soluble based upon the highest administered dose. In the case of diazepam, the drug itself is poorly soluble, but may be listed as a human BCS class I compound because of the low administered dose. The importance of considering dose was underscored with diazepam where our cited canine investigations used a dose of 40 mg (i.e., approximately 4 mg/kg). This is in contrast with a 10-mg dose in humans (i.e., approximately 0.14 mg/kg for a 70-kg person). Thus, although included in the list of BCS class I compound for this analysis, it would have been more appropriate to have classified diazepam as a BCS class II drug (at least for the sake of the canine investigation). Diazepam was in the lower right quadrant of the group of class I drugs (Fig. 2a), and considering the low solubility of diazepam, it is not surprising that its oral bioavailability was very poor in dogs where tablet dissolution is further compromised by a rapid GI transit time (vide infra).
Bcs Classification Database
The BCS classification is influenced by the ability of the highest dose strength to be fully solubilized in 250 mL (~ one cup) of aqueous media over the pH range of 1–7.5. However, for low solubility compounds, interspecies differences in absorbable dose may also be impacted by the composition of the GI fluids. In this regard, the unique composition of canine GI fluid can lead to differences in canine-human in vivo tablet dissolution ().
Because dissolution impacts oral bioavailability, it is important to distinguish between criteria used to evaluate the inherent solubility of the active pharmaceutical ingredient (API) versus that used to characterize in vivo dissolution of a dosage form. As compared to an assessment of the API, the dissolution rate (DR) of any formulated product is a function of its available surface area (A), the diffusion coefficient (D) of the drug (i.e., its ability to move from the undissolved portion of the API to the surrounding dissolution medium, the effective boundary layer thickness (h, which is the water that physically surrounds the undissolved API), the saturation concentration of the API under the conditions of the dissolution test (Cs), the amount of drug already dissolved (Xd), and the volume of fluid (V) within which the dissolution must occur (). From an interspecies perspective, differences in GI fluid volume and composition can have an effect on most of these variables. These interrelationships are described by the Noyes-Whitney equation ():
These considerations will be particularly important for low solubility compounds and may further complicate efforts to generate interspecies comparisons based upon the bioavailability of solid oral dosage forms.
Another challenge facing an examination of canine BCS criteria is that of defining what constitutes a high versus low permeability compound. Because there are no commercially available canine cell lines (), in the absence of in vitro permeability data, we have relied upon LogP values as the basis for estimating a canine BCS permeability cutoff value. Our selection of LogP values was founded upon published reports where LogP was used as a surrogate for human permeability studies (–). These referenced studies used metoprolol, with a LogP = 1.72 as the reference standard for the cutoff between high/low permeability. Drugs with LogP > 1.72 are classified as highly permeable, while those with LogP < 1.72 are classified as low permeability (, ). Our literature search did not produce any canine pharmacokinetic data for oral metoprolol. However, we did have information on a similar β-adrenergic antagonist, bisoprolol, which has chemical characteristics similar to that of metoprolol (BCS class 1, low Do, and LogP 1.94) and greater than 90% oral absorption in dogs (), suggesting that we could rely upon the human LogP cutoff of 1.72 for our canine assessments.
We failed to observe a correlation between a LogP cutoff value of 1.72 versus those drugs having high or low F values in dogs (Fig. 4). In fact, a line drawn at a LogP of 1.72 would practically split this group of drugs down the middle. That is, many drugs were found to be highly bioavailable (and therefore presumably highly permeable) whether or not they had LogP values above or below 1.72. Likewise, we identified several BCS class III drugs (high solubility, low permeability) with F values as high, or higher in dogs as compared to humans (Fig. 2c).
In the absence of first-pass drug loss, further study will help to determine whether or not the use of LogD (which is based upon both ionized and unionized species, i.e., is a pH-dependent value) rather than LogP would have been a more appropriate metric because LogD values better reflect the impact of GI pH on human-canine permeability differences. For compounds with molecular weights ranging from 165 to 644, the relationship between the Caco-2 cell-based apparent permeability (Papp) and LogD values were described by a bell-shaped relationship (). Highly permeable compounds (i.e., those with Papp values of 100–340 nm s−1) had LogD values ranging between 0 and 3, while low permeability compounds had values of either less than −1.5 or greater than 4.5. However, Kramer () observed that the reliability of LogD for estimating permeability appears to diminish when the molecular weight exceeds 500, and additional variables impacting permeability (e.g., hydrogen bonding properties, molecular size and shape, polarity, and flexibility) may need to be examined.
When considering the compounds where we have identified dog-human disparities in F, presystemic drug metabolism is likely to be an important factor to consider. This was seen in the drugs that fell below the line of unity in Fig. 2a–d, where several of these agents are known to be highly metabolized in dogs. There are also compounds (cyclosporine, carvedilol, dolasetron, and diltiazem) that were associated with high first-pass drug loss but had similar human-canine values of F. Therefore, an identification of pathways (e.g., CYP450 metabolizing enzymes, uptake and efflux transporters) responsible for the presystemic drug loss may help predict those drugs for which there is likely to be interspecies bioavailability differences.
Presystemic drug loss is a likely reason for some of the differences in the interspecies relationship described by Chiou et al. () as compared to that reported in this current study. In particular, canine oral bioavailability in this study was either similar to or lower than that reported by Chiou and colleagues. They () reported values based upon urinary concentrations of total drug, but the studies used in our analysis analyzed only the parent compound, typically using HPLC methods. We believe that the trend toward lower bioavailability in our dataset likely reflects differences in gut or hepatic presystemic metabolism in the dog.
Although one ordinarily anticipates a low F for poorly permeable drugs, there were two BCS class III and IV compounds with human F > 0.90 (amoxicillin and cephalexin). Despite their poor membrane permeability, both compounds undergo active transport via peptide transporter 1 (PEPT1) (–). Thus, enterocyte penetration via facilitated/active rather than passive processes will result in an extent of absorption that cannot be predicted solely on the basis of BCS classification criteria. Moreover, numerous BCS class III and IV compounds were associated with an F > 0.80 in dogs but not in humans. It is undetermined why these drugs defined as poorly permeable exhibited such high F values in dogs. Because the dog intestine is anatomically shorter than that of humans, in order to absorb nutrients, the canine intestine may have evolved a greater capacity for intestinal uptake transport as compared to that of humans. Less active intestinal efflux transport also is possible. For low molecular weight compounds, there is also greater paracellular absorption for some compounds in dogs than humans () (vide infra).
For furosemide, there was higher bioavailability from a 400-mg dose (F 0.77) compared to a tenfold lower dose of 40 mg (F 0.38). Class III and IV drugs ordinarily typically do not exhibit saturable drug efflux (). But for this class IV compound, efflux transport apparently can be saturated at high doses, thus increasing its oral bioavailability (–). Therefore, it would seem likely that at the high doses of furosemide administered in the canine study, an increase in enterocyte concentrations produced a saturation of efflux transporters and a corresponding larger F.
When drugs with relatively high F values in dogs were considered (Fig. 5), most of those compounds were associated with LogP values >0. The only drugs in this study that showed both high F values in dogs and LogP < 0 were gabapentin, amoxicillin, metronidazole, and theophylline—all class III drugs that were in the upper right quadrant of Fig. 2c. In these cases, the high F in dogs, despite low LogP, can be explained by other factors. Gabapentin and amoxicillin rely on intestinal influx transporters for their absorption. Metronidazole and theophylline are small molecules (molecular weight 171 and 198, respectively) that can be absorbed via paracellular pathways. Drugs of low molecular weight are likely to be absorbed from the intestine via the paracellular pathway rather than by transcellular diffusion. Dogs have larger pore size and a greater frequency of pores in the intestine compared to that observed in other species (). This difference in pore number and diameter may have contributed to the observed greater oral absorption irrespective of the compound’s Peff value. Furosemide is another example of a drug for which paracellular absorption has a significant impact (, ) and where the differences between F in humans and dogs may reflect the competing effects of paracellular versus transcellular absorption and efflux transport of those molecules that did successfully enter into the enterocyte.
Some of the BCS class III compounds such as morphine and codeine (high solubility, low permeability) had lower F in dogs than in humans (Fig. 2c). For these compounds, the marked interspecies difference in oral bioavailability is the result of a high first-pass metabolism in dogs (, ), a characteristic of oral opiates in dogs that is not as prominent in humans. Other oral opiates not included in this analysis also have essentially zero oral systemic availability in dogs (, ). For these drugs, systemic clearance exceeds liver blood flow and there may be extrahepatic metabolism contributing to the high first-pass metabolism.
For lipophilic compounds (BCS class II and IV), solubilization can be significantly impacted by bile salt composition and excretion. If the bile salt-drug interactions result in micelle formation, the resulting encapsulation can lead to a decrease in drug transport, limiting the ability of free drug to move across a biological membrane (). The formation of micelles can either increase or decrease drug absorption, depending upon the magnitude of its impact on solubility versus permeability (). A micellar-induced increase in the solubility of lipophilic compounds (due to endogenous, food-associated, or formulation-associated surfactants) can increase or decrease drug intestinal permeability () by reducing the partition coefficient between the intraluminal fluid and the biological membrane (). Thus, the pH and composition of GI fluids can be pivotal to dog-human differences in the absorption of lipophilic molecules.
The analysis presented in this paper reveals some challenges and pitfalls of relying on the human BCS parameters to predict performance of oral drug products in dogs. Because the BDDCS also takes into consideration presystemic drug metabolism, the combination of the BCS and BDDCS criteria for evaluating oral drugs in dogs may be a better approach to examine human/canine differences in oral bioavailability than the use of a single classification system. This approach is consistent with the perspective explained by Shugarts and Benet () where they note that the BDDCS considers the major route of elimination as an important factor in classification instead of permeability. As emphasized by Shugarts and Benet (), “BCS cannot predict absorption,” which is what we observed in this study. The BDDCS divides drugs into four classes based on solubility (high or low, as in the BCS), and whether or not the drug has low, or extensive metabolism. Because permeability data is difficult to acquire for medications in dogs, and because the LogP reference values used to assess human GI permeability do not appear to predict oral absorption for dogs, a system such as the BDDCS or some new system for dogs should be explored.
We are continuing in our effort to examine the specific factors that explain the observed human-canine differences in oral drug absorption. When considering sources of potential interspecies divergence, the important physiologic variables include GI fluid pH and composition, intestinal transit time, mucosal surface area, and the size and density of intestinal intercellular pores (–). These factors are particularly influential in the absorption of low solubility and/or low permeability drugs and may be helpful to predict interspecies differences in food effects (). Further considerations into metabolic pathway and influx/efflux transporter activity needs to be incorporated into our overall assessment. It is with these points in mind that we have summarized the important variables to incorporate into our human-canine interspecies extrapolations (Table II).
CONCLUSION
This investigation showed that applying the same BCS criteria to dogs and humans can be problematic. At least in part, when attempting to designate a BCS classification for dogs, there is a need to develop canine-specific solubility and permeability assessments. Ultimately, even when the necessary in vitro methods for estimating canine drug solubility and permeability have been developed, canine-human physiological differences can result in marked differences in systemic absorption due to transporter functions, drug metabolism, and the leakier canine intestinal membranes.
Clearly, there remains much work to be done in order to improve our ability to predict drug absorption in the dog when based upon preliminary drug physicochemical characterization and an interspecies extrapolation of in vivo PK information. Efforts to predict drug absorption (or to understand the causative factors impacting interspecies differences in F) is dependent upon a wide array of variables including API solubility and permeability (BCS), formulation factors, and physiological variables (including regional permeability differences, which could differ between species), GI pH, luminal and mucosal enzymology, and intestinal motility, first-pass drug metabolism, and transporter activity (–). It is for this reason that a blending of BCS and the BDDCS may provide far better predictions of canine versus human drug absorption characteristics than would either classification system alone. Comparing drug absorption characteristics in dogs and humans, while important for interspecies extrapolations and for formulation development, also provides valuable insights into the variables that can influence drug absorption (and interindividual differences) that can occur in the presence of human or canine GI pathologies, breed potential breed effects on canine drug absorption, or the changes in drug absorption that may occur in the geriatric dog or human population. Such predictions are predicated largely upon the development of mechanistic (in silico) models. By understanding the impact of these critical variables on the rate and extent of drug absorption, these models can be positioned for use in predicting the canine to human (and vice versa) differences in oral drug absorption and in vivo product performance.
Our ongoing efforts are based upon the use of this drug list to explore published human-canine differences in drug metabolism, along with an evaluation of other potential variables. We anticipate that through these efforts, we will obtain a better appreciation of the pivotal factors dictating in vivo product absorption and determine potential sources of error when attempting to extrapolate information obtained in humans to support in silico predictions of in vivo drug absorption characteristics in dogs.
At the time this manuscript was prepared, we did not have access to the paper published by Musther et al. (). Their paper included 125 paired datasets comparing F between dogs and humans and included many of the same studies that were used in our analysis. As we report here, they also found a poor correlation in F for drugs between dogs and humans with an R value of 0.37. Musther et al. () did not include BCS criteria in their analysis, but instead, separated compounds into acidic, basic, neutral, or zwitterions. This improved the prediction slightly for acidic drugs, some of which were likely BCS class II compounds. A prediction model of human F from canine values, based on a linear regression model, resulted in wide prediction intervals with a low concordance correlation coefficient (precision of the prediction), confirming the lack of agreement between human and dog F values. As in our studies, they found that Beagle dogs were represented more often than other dog breeds for bioavailability determination in most studies (66%). We encountered similar problems as described by Musther et al. () when extracting data from published studies. Some studies provided full details of the methods and results and others provided limited data. They concluded, as we did, that metabolic differences between species could play a more important role in defining disparities between human and animal drug bioavailability.
ACKNOWLEDGMENTS
The authors would like to thank Robyn Martinez for her help collecting data for this manuscript. They also appreciate the support from the United States Pharmacopeia in the early stages of this project. The authors also acknowledge the advice and recommendations from Dr. G.L. Amidon and Dr. James Polli in the analysis of these data.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Contributor Information
Mark G. Papich, Email: ude.uscn@hcipapgm.
Marilyn N. Martinez, Email: vog.shh.adf@zenitram.nyliram.
REFERENCES
Bcs Drug Classification
Abstract
BCS and BDDCS are complimentary, not competing, classification systems that aim to improve, simplify, and speed drug development. Although both systems are based on classifying drugs and NMEs into four categories using the same solubility criteria, they differ in the criterion for permeability and have different purposes. Here the details and applications of both systems are reviewed with particular emphasis of their role in drug development.
INTRODUCTION
The FDA’s Biopharmaceutics Classification System(BCS)1 is based on the work of Amidon and coworkers with the core idea being that in vitro methodology, centrally embracing permeability and solubility, with qualifications related to pH and dissolution, may qualify drug products for a waiver of in vivo bioequivalence studies. The objective of the BCS is to predict in vivo performance of drug products from in vitro measurements of permeability and solubility.
In 2005, Wu and Benet recognized that for drugs exhibiting high intestinal permeability rates the major route of elimination in humans was via metabolism, while drugs exhibiting poor intestinal permeability rates were primarily eliminated in humans as unchanged drug in the urine and bile. They proposed that a biopharmaceutics drug disposition classification system (BDDCS) could serve as a basis for predicting the importance of transporters in determining drug disposition, as well as in predicting drug-drug interactions.
The major differences between BCS and BDDCS relate to their purpose and the measurement for classification as depicted in Table 1. The purpose of BCS is to characterize drugs for which products of those drugs may be eligible for a biowaiver of in vivo bioequivalence studies. The purpose of BDDCS is to predict drug disposition and potential drug-drug interactions in the intestine and the liver, and potentially the kidney and brain. Both BCS and BDDCS use solubility as one of the two classification criteria. The solubility parameter utilized may be called the FDA solubility, that is, an estimate of the ability of the drug at its highest dose strength to completely dissolve in 250 ml of water over a pH range between 1 and 7.5 at 37°C. For a drug to be considered highly soluble in the two classification systems, the drug from its highest strength regulatory approved dosage form must go completely into solution at its lowest solubility over this pH range in 250 ml of water. As we have recently noted, FDA solubility is a property of the drug in a formulation and is not an intrinsic property of the active pharmaceutical ingredient itself. The second classification parameter, and where the two systems differ, is related to intestinal permeability. In BDDCS, predictions are based on intestinal permeability rate, which was found to be related to extent of drug metabolism. In BCS, biowaivers are based on the extent of intestinal absorption, which in a number of cases does not correlate with intestinal permeability rate.
Table 1
| BDDCS | BCS |
|---|---|
| Purpose | |
| Predicting drug disposition and drug-drug interactions in the intestine and liver | Facilitate biowaivers of in vivo bioequivalence studies |
| Criterion | |
| Predictions are based on intestinal permeability rate | Biowaivers are based on extent of intestinal absorption (permeability), which in a number of cases does not correlate with rate of jejunal permeability. |
THE BCS AND ITS USE IN DRUG DEVELOPMENT
The BCS characterizes drugs into four classes according to their FDA solubility and permeability as depicted in Fig. 1. In 2000, the FDA promulgated the BCS system as a science-based approach to allow waiver of in vivo bioavailability and bioequivalence testing of immediate-release solid oral dosage forms for Class 1 high solubility, high permeability drugs when such drug products also exhibited rapid dissolution1. This waiver is based on a triple-tier rationale where: a) high solubility insures that drug solubility will not limit dissolution, and thus absorption, b) high permeability insures that drug is completely absorbed during the limited transit time through the small intestine, and c) rapid dissolution insures that the gastric emptying process is the rate-limiting step for absorption of highly soluble and highly permeable drugs. Drug sponsors are allowed to use mass balance, absolute bioavailability, or human intestinal perfusion studies to demonstrate high permeability1. The FDA Guidance, however, also recommends possible methods not involving human subjects including in vivo or in situ intestinal perfusion in a suitable animal model, and/or in vitro permeability methods using excised intestinal tissues or monolayers of suitable epithelial cells1,, usually the Caco-2 cell system. However, some studies have shown that in vitro cellular permeability criteria recognized in the FDA’s BCS guidance may not always correctly predict the extent of drug absorption in humans–.
The Biopharmaceutics Classification System (BCS) as defined by the FDA1 after Amidon et al.
In 2010, the European Medicine’s Agency (EMA) revised its bioequivalence guideline stating that demonstration of complete absorption in humans is preferred for biowaiver of BCS Class 1 drug applications rather than measures of high permeability9. The criteria for complete absorption in the EMA Guidline is ≥85% measured extent of absorption in humans based either upon absolute bioavailability or mass balance studies9.
The correlation between intestinal permeability rate and the extent of absorption in humans came from the results of in vivo studies with 34 drugs and endogenous substances, where a good correlation was observed between jejunal permeability from human intestinal perfusion studies and the fraction of the oral dose absorbed in humans. However, in these early human intestinal perfusion studies, no drugs were investigated that subsequently showed a discordance between cellular system permeability rates and the extent of absorption in humans. It is now generally recognized by the FDA, the EMA and the research scientists in the field that high cellular permeability rates do correctly predict a high extent of absorption. Discordance is essentially only found for some non-metabolized drugs exhibiting low cellular permeability rates but complete absorption.
The role of BCS in drug development is facilitating the possibility of obtaining a waiver of in vivo bioequivalence studies for drug products, where the regulatory agencies recognize the drug as BCS Class 1 and where the dissolution rate of the new drug product meets the rapid dissolution criteria of the regulatory agencies. This is definitely a simplifying and cost saving procedure in drug development. However, there is no predictive benefit to BCS. Studies in humans must be carried out to show that the drug achieves complete absorption (≥90% for FDA and ≥85% for EMA, although the FDA has indicated informally that ≥85% may be appropriate for a biowaiver). Yet, as stated above, cellular studies exhibiting high permeability rates can give sponsors confidence that a high solubility compound will meet the extent of absorption criteria of the regulatory agencies prior to obtaining actual extent of absorption measures in humans. Since the promulgation of the FDA BCS Guidance in 2000, a number of new possible class boundaries have been proposed for additional biowaivers. For example, the EMA will grant biowaivers for BCS Class 3 drugs with high solubility but limited absorption9. In addition, a World Health Organization (WHO) Technical Report11 suggests that biowaivers may be appropriate for so-called BCS Class 2a drugs, weak acids that exhibit low solubility only at low pH. The WHO recommended criteria for such drug products would be rapid dissolution at pH 6.8 and a similar dissolution profile to the innovator product at pH 1.2, 4.5 and 6.8. Like the EMA, the WHO Technical Report also recommends biowaiver eligibility for Class 3 very rapidly dissolving drug products that contain no inactive ingredients that are known to alter GI motility and/or absorption11. However, at this time only BCS Class 1 drugs are eligible for a biowaiver of in vivo bioequivalence from the FDA1 and BCS Class 1 as well as some Class 3 drugs by the EMA9.
BDDCS
As described above the purpose of BDDCS is to predict drug disposition and potential drug-drug interactions in the intestine and the liver with an emphasis on defining which drugs would be amenable to enzymatic-only and transporter-only disposition and drug-drug interactions, as well as where transporter-enzyme interplay may be important. Recent reviews from the Benet Lab– have defined these enzymatic, transporter and transporter-interplay characteristics with potential transporter effects following oral dosing as depicted in Figure 2. The recognition of the correlation between BCS intestinal permeability and BDDCS extent of metabolism by Wu and Benet preceded an explanation for these findings. We hypothesize now that high permeability rate compounds are readily reabsorbed from the kidney lumen and from the bile, facilitating multiple access to the metabolic enzymes. For example, consider the BCS/BDDCS Class 1 drug letrozole. This completely oral available drug is primarily eliminated by metabolism via CYP3A4 and CYP2A6 enzymatic processes with less than 4% of the dose excreted unchanged in the urine. However, letrozole is only 60% bound to plasma proteins and thus it might be expected, based on glomerular filtration rate and fraction unbound, that renal clearance could approach 48ml/ml. Yet the total clearance for letrozole is only 40.5 ml/min with less than 4% excreted unchanged. Thus, this high permeability compound is reabsorbed in the kidney tubules (and possibly from the bile) with the major route of elimination being metabolic processes. The rationale for the correlation between intestinal permeability rate and the extent of metabolism appears to be based on the fact that high permeability rate compounds are reabsorbed from potential unchanged drug excretion routes in the body and thus can only be eliminated through metabolism. This hypothesis, then led us to conclude that the measure of high permeability rate in making the BDDCS assignment need not necessarily be a human biological membrane or membrane surrogate, but that passive permeability in any appropriate membrane model may provide the correct assignment. This topic will be discussed further below.
Transporter effects predicted by BDDCS following oral dosing.
THE USE OF BDDCS FOR DRUGS ALREADY ON THE MARKET
Table 2 lists six potential uses of BDDCS in characterizing drugs that have already reached the market. The text below provides greater detail for each of these six potential uses.
Table 2
|
For drugs already on the market, BDDCS provides potential predictability of drug-drug interactions that had not been anticipated or tested in the drug approval process. For example, our laboratory recognized that atorvastatin was a BDDCS Class 2 drug exhibiting extensive metabolism and poor solubility. Thus, as shown in Fig. 2, we recognized that atorvastatin may potentially exhibit a drug-drug interaction with inhibitors of hepatic uptake transporters. We first demonstrated in cellular and isolated perfused rat liver studies that atorvastatin, as well as its two active hydroxylated metabolites, were substrates for human and rat OATPs and that inhibition of OATP uptake would decrease atorvastatin metabolism. We then carried out whole animal studies in rats to confirm this finding in intact animals. We then demonstrated in healthy volunteers that a single intravenous dose of rifampin, a potent OATP inhibitor would significantly increase the total AUC of atorvastatin acid by 6.8±2.4-fold and that of 2-hydroxy-atorvastatin acid and 4-hydroxy-atorvastatin acid by 6.8±2.5-fold and 3.9±2.4-fold, respectively. Of course, once recognizing that atorvastatin and its active metabolites are substrates for OATP1B1, then it would logically follow that genetic variants in this transporter would affect atorvastatin pharmacokinetics, as has been demonstrated. Thus, BDDCS is also useful in predicting where pharmacogenetic variants can yield meaningful drug disposition changes.
In a further study we demonstrated that inhibiting the hepatic uptake transporter for glyburide would also significantly increase its area under the curve and that blood glucose levels were lower than those observed after dosing with glyburide alone. Glyburide is primarily a substrate of OATP1B3, which does not exhibit significant changes in activity with genetic variants, and therefore one would suspect that a pharmacogenetic study of the transporter would not yield significant changes. However glyburide is a substrate for CYP2C9, with known disposition changes for the genetic variants of this enzyme.
It is important to recognize that the BDDCS characterization of transporter effects, and transporter enzyme interplay as depicted in Fig. 2 does not predict that every drug in each class will display the effects listed. Rather, BDDCS predicts what transporter effects may occur, and which may not, and what should be tested. As an example, the Class 2 drug felodipine is a CYP3A substrate, but not a substrate for P-glycoprotein, and we used it as our control in examining Class 2 drug efflux transporter-enzyme interplay. Furthermore, one cannot be sure that a cellular transporter-enzyme interaction will translate into an in vivo clinically relevant interaction, even when the in vitro Ki values suggest that the interaction needs to be tested. As an example, numerous publications concerning the pharmacogenomics of warfarin have shown that accounting for the genetic variants of CYP2C9 and VKORC1 plus other patient parameters can only explain about 55% of the variability observed for this drug in patient populations. Since warfarin is a Class 2 drug, we asked could it be a substrate for an uptake transporter, and if so might knowledge of this transporter genotype increase the predictability? Rat and human hepatocyte studies showed that warfarin appeared to be a substrate for OATP uptake that could be inhibited by rifampin, which might account for an ~30% change in AUC. The in vitro interaction was of the same magnitude as what we had observed in vitro for glyburide. We then carried out a human study that showed that there was no significant increase in warfarin blood concentrations in the presence of the OATP inhibitor rifampin.
Recently the FDA has recommended that studies in renal failure patients be carried out even for drugs where renal elimination of unchanged drug is minimal23. This recommendation comes about in part based on a finding that was related to the development and characterization of BDDCS. Previous studies of changes in drug metabolism in renal failure patients for drugs primarily eliminated by hepatic metabolism were thought to be related to the effects of uremic toxins as either potential inhibitors or down regulators of metabolic enzymes. However, this could be tested in vitro and was shown not to occur in many cases. We began to recognize that previously unexplained effects of renal disease on hepatic metabolism can result from accumulation of substances (toxins) in renal failure that modify hepatic uptake and efflux transporters–, and that this mechanism could explain why BDDCS Class 2 drugs could demonstrate changes in metabolism in renal failure, while this would not be observed for BDDCS Class 1 drugs when in vitro uremic toxins did not alter microsomal metabolism.
To demonstrate the relevance of the potential effect of uremic toxins in patients we compared the pharmacokinetics of oral and IV erythromycin in patients with end stage renal disease versus healthy volunteers. Erythromycin is a BDDCS Class 3 drug that is primarily eliminated unchanged in the bile. It is a substrate for hepatic uptake transporters that we had previously shown can be inhibited by uremic toxins. We demonstrated that the hepatic clearance of erythromycin in end stage renal disease patients was decreased by 31% (p=0.01) and that bioavailability was increased 36%. Since we had given the drug both intravenously and orally, we calculated that there was no change in the fraction of the oral dose absorbed multiplied by the potential gut availability (Fabs·Fg). This would be expected even though erythromycin, a Class 3 BDDCS drug is a substrate for an intestinal uptake transporter, since it is not possible for the uremic toxins to be present in the intestine. Thus the BDDCS allows investigators to predict the potential effect of uremia on hepatic metabolism and biliary excretion.
To facilitate use of the BDDCS system for making predictions for drugs on the market, we recently compiled the BDDCS classification for 927 drugs, which include 30 active metabolites. Of the 897 parent drugs, 78.8% (707) are administered orally. Where the lowest measured solubility was found in the literature this value was reported for 72.7% (513) of these orally administered drugs. Measured values are reported for the percentage excreted unchanged in the urine, Log P and Log D 7.4, when available. For all 927 compounds the in silico parameters for predicted Log solubility in water, calculated Log P, Polar Surface Area and the number of hydrogen bond acceptors and hydrogen bond donors for the active moiety are also provided, thereby allowing comparison analyses for both in silico and experimentally measured values. We showed that when comparing the in silico parameters across the four classes, there is a distinct difference between Class 2 and Class 3 compounds. However, surprisingly the Log P and solubility in silico parameters for the Class 1 drugs appear to be intermediate between those for Class 2 and Class 3 and not very different than the parameters for the Class 4 drugs. We note this failure of in silico parameters to efficiently predict whether a drug will be Class 1, believed by many to be the most desirable due to high solubility and high permeability, versus Class 4 drugs that are low solubility and low permeability.
Most recently we have shown that the prediction of brain disposition of orally administered drugs may be improved using BDDCS. It is generally believed that high Log P, high permeability and lack of P-gp efflux are desirable characteristics for CNS drug candidates to become marketed CNS drugs–. From the literature we were able to identify 153 marketed drugs that met three criteria: a) central or lack of central pharmacodynamics effects were known; b) the BDDCS class was identified; and c) information was available as to whether the drug was or was not a substrate for P-glycoprotein. About 98% of BDDCS Class 1 drugs were found to be markedly distributed throughout the brain; this includes 17 BDDCS Class 1 drugs known to be P-gp substrates. Thus, we expand upon the transporter effects listed in Fig. 2 for Class 1 drugs. We now believe that transporter effects are minimal, and clinically insignificant, for Class 1 drugs in the gut, liver and brain, and suspect that this is also true for the kidney. Recognition that BDDCS Class 1 drugs that are P-gp substrates will still yield central effects allowed us to decrease the number of compounds incorrectly predicted from in silico parameters in terms of disposition from the 19–23% employing previous methods,, to less than 10%. This finding of a lack of a clinically significant effect of P-gp on brain disposition of BDDCS Class 1 drugs has marked implications for predicting drug disposition and effects of NMEs, as will be described in the last section of this report.
Finally, there is also an application to BCS biowaivers inherent in the BDDCS Classification System. Benet and coworkers recognized that for 29 drugs where measured human intestinal permeabilities were available, the extent of metabolism correctly predicted high versus low permeability for 27 of 29 (or 93%) of the measured human intestinal permeabilities in terms of BCS. Thus, Benet and colleagues recommended that regulatory agencies add the extent of drug metabolism (i.e., ≥90% metabolized for FDA and ≥85% metabolized for EMA) as an alternate method for determining the extent of drug absorption in defining Class 1 drugs suitable for a waiver of in vivo studies of bioequivalence. The authors propose that the following criteria be used to define the ≥90% metabolized for FDA marketed drugs: “Following a single oral dose to humans, administered at the highest dose strength, mass balance of Phase I oxidative and Phase II conjugative drug metabolites in the urine and feces measured as either unlabeled, radioactive labeled or non-radioactive labeled substances, account for ≥90% of the drug dose. This is the strictest definition for a waiver based on metabolism. For an orally administered drug to be ≥90% metabolized by Phase I oxidative and Phase II conjugative process it is obvious that the drug must be absorbed.” In their 2010 revised bioequivalence guidance9, EMA incorporated this recommendation. FDA scientists have also supported this recommendation, although no formal written guidance change has been issued.
THE ROLE OF BDDCS IN THE DRUG DEVELOPMENT OF NEW MOLECULAR ENTITIES (NMEs)
Although BDDCS can be used for characterizing disposition of drugs already on the market, as detailed in Table 2 and in the text above, the goal of BDDCS was to predict and characterize drug disposition for new molecular entities. Table 3 lists those uses and the text below is a prescription for utilizing BDDCS with NMEs.
Table 3
Additional Uses of BDDCS for New Molecular Entities and its Role in Drug Development
|
For an NME it would be most useful to predict its BDDCS class prior to any studies in humans, animals or even cellular systems. The recognition of the correlation between intestinal permeability rate and extent of metabolism allows prediction of BDDCS class for an NME to be based on passive membrane permeability35. Initially we proposed to follow the BCS permeability rate measure in the Caco-2 cellular system using metoprolol, but now more preferably labetalol, as the cutoff between high and low permeability compounds. However, since we now believe that it is the passive permeability that is the predictive parameter, we suggest that even studies with an artificial membrane such as PAMPA will provide a reasonable prediction of BDDCS Class 1 and 2 versus BDDCS Class 3 and 4 using labetalol as the cut off marker. We evaluated35 the permeability results for 21 drugs studied by three different PAMPA models (a lipid/oil/lipid tri-layer, a bio-mimetic, and a hydrophilic filter membrane PAMPA assay). For these 21 drugs the human extent of absorption and metabolism was known. In this evaluation the extent of absorption or metabolism was defined as being low or high if it was less than 30% or ≥90%, respectively. Permeability was defined as being low or high if it was less than 2.0 or ≥3.5x10−6cm/s, respectively based on a marked differentiation using these cut-offs for 19 of the 21 drugs. The high PAMPA permeability for all three models accurately predicted BCS ≥90% absorption very well and only slightly less accurately BDDCS metabolism. However, for low PAMPA permeability while the system very accurately predicted poor BDDCS metabolism the systems only correctly predicted absorption 25% of the time. Based on these data we suggest that passive transcellular drug permeability in an artificial membrane may reasonably predict extensive versus poor human metabolism35. Note that we are not suggesting that the permeability rate cut offs listed above are numbers that may be translated to other laboratories. They are just the values from our in vitro permeability rate analyses used to attempt to differentiate the 21 drugs for which human in vivo permeability rate measures and extent of metabolism have been reported.
Although we believe it is quite easy, and using high throughput methods, to predict with good accuracy Class 1 and Class 2 versus Class 3 and Class 4 assignment of an NME, it is not easy to differentiate high solubility from low solubility. The major impediment is that the BDDCS (and BCS) solubility criterion is based on the highest marketed dose strength. Of course, for an NME such knowledge may be years away from the compounds initial evaluation. Therefore we propose following the recommendation of Pfizer scientists to use a solublity cutoff of 200μg/ml (i.e., 50 mg highest dose strength) in the initial evaluation. Thus, compounds with a lowest solubility over the pH range 1–7.5 being greater than 200μg/ml would be assigned Class 1 or Class 3 and those with a lowest solubility less than 200μg/ml would be assigned Classes 2 and 4. As we have noted previously, in silico predictions of solubility are not very reliable and thus we also recommend following the Pfizer protocol of utilizing a high throughput equilibrium solubility assay for NMEs in simulated gastric fluid at pH 1.2 and in 50 mM phosphate buffer pH 6.5, for the initial assignment. Thus, very early in the drug development of an NME, using only in vitro methods to assign BDDCS class, sponsors will be able to predict the major route of elimination of an NME in humans (metabolism versus excretion of unchanged drug in the urine and bile) and predict the relevance of transporters and transporter-enzyme interplay in drug disposition. If an NME is BDDCS Classes 1 or 2, the drug should exhibit good absorption, but not necessarily good bioavailability. In contrast, if the NME is BDDCS Classes 3 or 4, then good absorption will only be achieved if the NME is a substrate for an intestinal uptake transporter or possibly small enough to pass through intestinal pores.
There is a marked difference in the BDDCS class distribution of drugs on the market as opposed to NMEs. We previously estimated the distribution for NMEs based on all recently synthesized medicinal compounds. In Fig. 3 we depict the distribution of oral immediate release drugs on the market versus small molecule NMEs, the latter percentages determined from a data set of Professor Oprea37 encompassing 28,912 medicinal chemistry compounds tested for at least one target and having affinities of μM or less concentrations. While 40% of oral immediate release marketed drugs are Class 1, only 18% of NMEs fall in this category. This difference is primarily related to Class 2 drugs, where 33% of marketed oral immediate release products are found versus 54% of NMEs. As can be seen in Fig. 3 quite similar numbers between marketed drugs and NMEs are found for Classes 3 and 4. That is, in essence, NMEs are becoming larger, more lipophilic and less soluble, with time in the drug discovery paradigm.
Distribution of 698 oral immediate release drugs on the market and NME percentages from a data set of 28,912 medicinal chemistry compounds tested for at least one target and having affinities at μM or less concentrations37 using BDDCS criteria.
Early characterization of the BDDCS class of an NME offers information related to of all those characteristics listed in Table 2 for drugs on the market. Of particular relevance, early in drug development, may be the information related to potential brain distribution as described in our recent publication. That is, if central effects for an NME are not desired, then a BDDCS Class 2 compond that is a substrate for brain efflux transporters would be preferable to a highly soluble BDDCS Class 1 NME. On the other hand, sponsors should recognize that if the NME was, in fact, BDDCS Class 1, then brain distribution and potential central off-target effects can not be avoided even if the compound is shown to be a substrate for brain efflux transporters.
BDDCS classification may also allow predictions regarding food effects for orally dosed drugs. The area under the curve (AUC) and bioavailability of many drugs are greatly affected by concomitant food intake and the FDA recommends that high fat meals (800–1000 cal; 50–65% from fat, 25–30% from carbohydrates, 15–20% from protein) may be used in food effect studies in humans38. Many factors are believed to contribute to these food effects, including changes in gastric emptying time, bile flow, pH of the intestine, splanchnic blood flow, and gut wall metabolism. A variety of evidence exists supporting food effects on transporters as well, as described by Custodio et al. In general high fat meals have no effect on the extent of absorption of BDDCS Class 1 drugs, increase AUC for BDDCS Class 2 drugs, decrease AUC for BDDCS Class 3 drugs, with insufficient data to show a general trend for Class 4 drugs. However, the multiplicity of factors affecting absorption in the presence of food make it more difficult to have a uniform response, and I estimate that the accuracy of the food effect predictions above is only approximately 70%.
SUMMARY
It is now been 17 years since Amidon et al. published the theoretical basis for the BCS. According to ISI this paper has now been referenced more than 1,350 times and is the most highly cited paper in the pharmaceutical sciences. The impact of this paper has been substantial leading to an FDA guidance1 and as befits the high citation rate, the paper has led to many other discoveries in the pharmaceutical sciences. Today all new drugs approved by the FDA and the EMA contain information related to the BCS classification of the molecule and its drug product. Although the purpose of BCS is to characterize drugs for which products of those drugs may be eligible for a biowaiver of in vivo bioequivalence studies, there is no inherent predictability of this characteristic, since the categorization is based on experimental results. This simple categorization of drugs into four classes has spawned many further approaches in drug product analysis. BDDCS is one of those derivative approaches. Wu and Benet recognize that the great majority of BCS Class 1 and 2 drugs were eliminated in humans predominantly by metabolic processes, while the great majority of BCS Class 3 and Class 4 drugs were predominantly eliminated unchanged either in the urine or bile. In the seven years since the BDDCS publication, it has also received a significant citation history, now close to 350. BDDCS was developed with the purpose of predicting drug disposition and drug-drug interactions, both for drugs on the market and NMEs. Very recently, Professor Amidon has characterized the 2005 BDDCS paper as advancing and conceptualizing “a new era of molecular ADME”. He has very graciously written, “I believe this 2005 BDDCS paper is a seminal concept in development in the field of molecular ADME of drugs and will have a profound impact on drug discovery and development in the 21st century, and, eventually human health and quality of life.”. I certainly hope that he is correct and in this commentary have attempted to lay out the significant role that BCS has played in drug development and the potential for the role that BDDCS may play.
Acknowledgments
I am very appreciative of the outstanding students, postdoctoral scholars and scientific collaborators who have worked with me over the years in developing the concepts of BDDCS and its role in drug development as presented here, as well as Professor Amidon and his coauthors who provided the basis for our work. Dr. Benet was supported in part in the preparation of this commentary by NIH Grant GM-061390.
Abbreviations used
| BCS | biopharmaceutics classification system |
| BDDCS | biopharmaceutics drug distribution classification system |
| EMA | European Medicines Agency |
| OATP | organic anion transporting polypeptide |
| NME | new molecular entity |
| PAMPA | parallel artificial membrane permeability assay |
| AUC | area under the curve |
References
Most Viewed Pages
- Warriors Orochi 3 Crystal
- Grundig Manual Download
- Resident Evil 0 Remastered Walkthrough
- My Serial Number
- Desene Animate Cu Printese In Limba Romana
- Activation Code For Autocad 2016
- Youtube Etv Daily Serials
- Xmovies8
- Star Jalsha Gillitv
- Paket Murah Telkomsel 2018
- Youtube Etv Daily Serials
- Nonton Film Gratis
- Que Aprendiste Quizlet
- Harry Potter 4 Full Movie
- Pagalworld Hd 2018
- Ramleela Songs
- Adobe Lightroom Download With Crack
- Solidworks 2014 Download Free
- Saint Seiya Episode Guide
- Product Key For Windows 7